Makena Dyck, Year 2 Research
Abstract
Many factors such as antibiotics, affect the immune systems function, while plant extracts, vitamins and minerals all support healthy function. This paper explores an Immune Blend consisting of vitamins C, E, D, zinc, iron, oregano oil and echinacea. The Immune Blend was tested alongside an antibiotic, streptomycin, in hopes of determining antibacterial properties of
the Immune Blend and the relationship between the two. This study found that the Immune Blend has antibacterial properties, but does not significantly boost the function of the antibiotic. However, these results are not enough to form solid conclusions due to certain limitations and possible sources of error. Though antibacterial properties were found, further experimentation and variable adjustments are needed to establish a solid conclusion.
Introduction
The adverse effects of antibiotics on the immune system are a worsening problem due to overprescription and antibiotic resistance (Spellberg and Hansen 2020). Antibiotics can directly affect the immune system by reducing the ability of immune cells to kill bacteria (Zusi 2017).
The benefits of natural oils and plants are used by 75% of the world’s population to treat viral and bacterial infections (Pan et al 2014). Studies show that many plant extracts, such as Oregano have antibacterial properties and can be effective against gram-negative bacteria (Masoon et al 2007). Furthermore, vitamins and minerals are a crucial aspect of the human diet and play an important role in the immune system. Vitamins aid the immune system in many ways: acting as an antioxidant to protect healthy cells, supporting the growth of immune cells and producing antibodies (Chandra 1997). Additionally, studies find that people with vitamin deficiencies and weakened immune systems are at greater risk of bacterial, viral and other infections (Ask the Expert: The Role of Diet and Nutritional Supplements during COVID-19).
This paper focuses on the potential antibacterial effects of an Immune Blend in combination with an antibiotic. Specifically, the Immune Blend is composed of plant extracts (oregano oil and echinacea), vitamins (vitamins C, E and D) and minerals (iron and zinc). Additionally, the ingredients in this blend were selected based on previous research of antibacterial properties and known importance and benefits to the immune system. The Immune Blend is being tested for antibacterial properties because the ingredients are known to have a positive impact on the immune system itself, but the direct antibacterial effects of the blend are unknown. Accordingly, the Immune Blend was tested alone and in combination with an antibiotic (streptomycin), on the gram-negative bacteria Escherichia coli (E.coli). The results of this paper impact the medical research field by creating a potentially alternative for antibiotics used to treat minor bacterial infections, if the right Immune Blend ratio is achieved.
Materials and Methods
Plate preparation
Prepare plates by pouring 1/2cm of LB agar into six Petri dishes. The upper left quarter was labelled ‘Control’, the upper right quarter ‘Antibiotic’, the lower right quarter ‘Immune Blend’ and the lower left quarter ‘Antibiotic+Immune Blend’. The bacteria used was indicated (E.coli), name and the date the plate was prepared. Additionally, the ‘group’ was indicated.
Figure 1: Example of correct plate set up
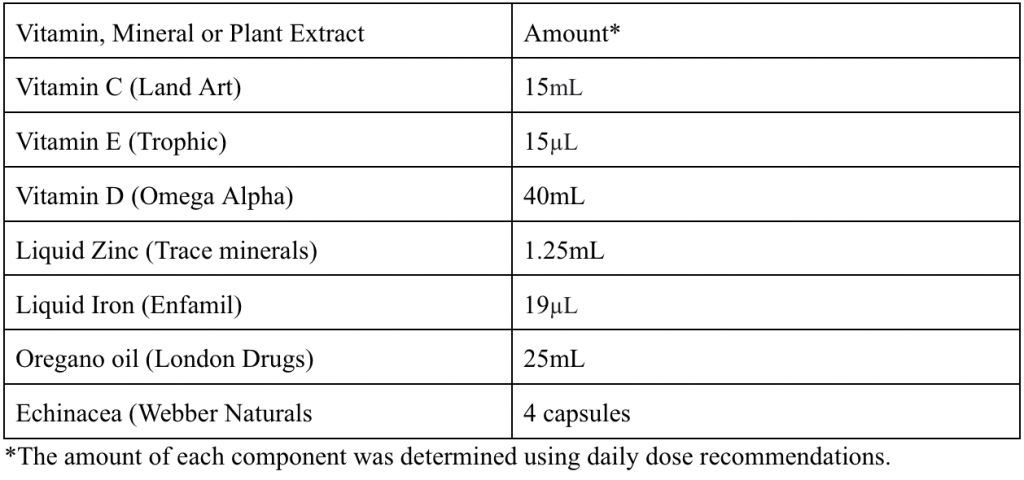
Immune Blend Preparation
The blend was prepared by measuring the indicated amount of each vitamin or mineral, and adding it to a beaker. 2 filters were placed in a funnel over a bottle to remove any chunks. The mixture was stored in a tightly sealed bottle and shaken well before use.
Table 1: Components of Immune Blend
Preparation of the first three plates
The plates labelled groups 1-3 followed this procedure for preparation. 100µL of 1:100 serially diluted E.coli was pipetted into a petri dish and was distributed using an L spreader. After the plate dried, a streptomycin tablet (Fisher Scientific) was placed in the second quarter. A sterilized tablet (Fisher Scientific) was soaked with 250 µL of Immune Blend and placed in the third quarter. A streptomycin tablet was soaked 250 µL of Immune Blend and placed in the fourth quarter. The petri dish was then closed, turned upside down and stored in an incubator.
Preparation of the final three plates
The plates labelled groups 4-6 followed this procedure for preparation. 100µL of 1:100 serially diluted E.coli was pipetted into a petri dish and was distributed using an L spreader. After the plate dried, a sterilized tablet with 250 µL of distilled water was placed in the first quarter. This
ensured that the effects of the Immune Blend were true and not due to flooding. A streptomycin tablet was placed in the second quarter. A sterilized tablet soaked with 250 µL of Immune Blend was placed in the third quarter. A streptomycin tablet was soaked 250 µL of Immune Blend and placed in the fourth quarter. The petri dish was then closed, turned upside down and stored in an incubator.
Incubation period
The plates were left upside down in the incubator for one week. After one week, the zones of inhibitions were recorded and observations were taken.
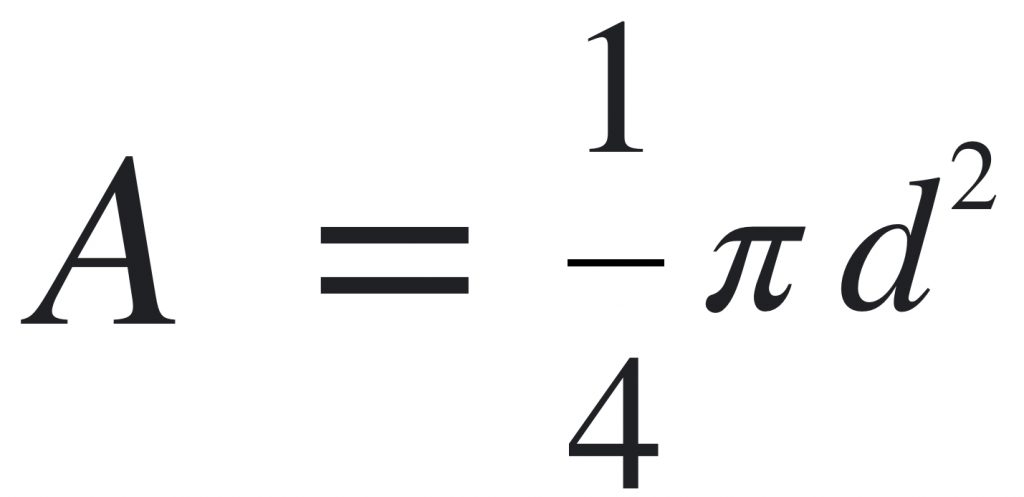
Determining the zone of inhibition
The zone of inhibition indicates the area where the antibiotic, Immune Blend or a combination of both killed bacteria. Usually, the zone of inhibition presented as a circle or oval, so the diameter was recorded and used to calculate the area of the zone of inhibition with the following formula:
Results
*Group indicates which trials were produced on the same petri dishes
Table 2: Antibiotic Trials
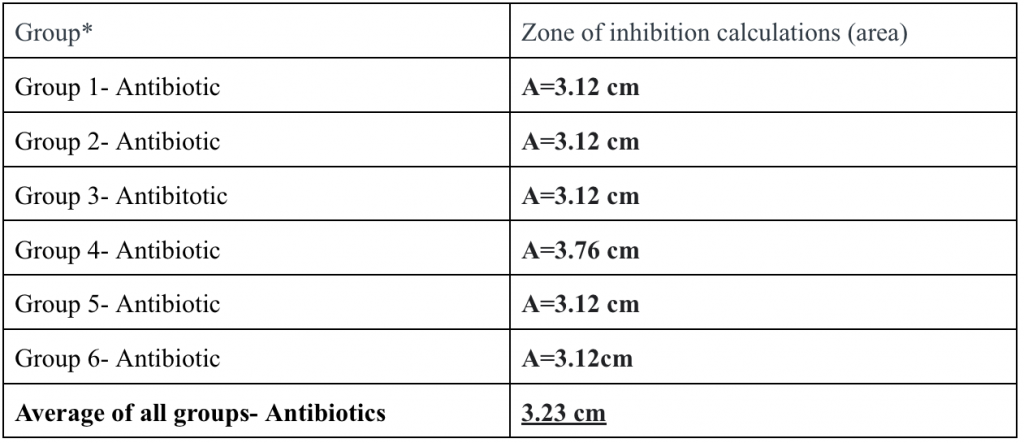
Table 3: Immune Blend Trials
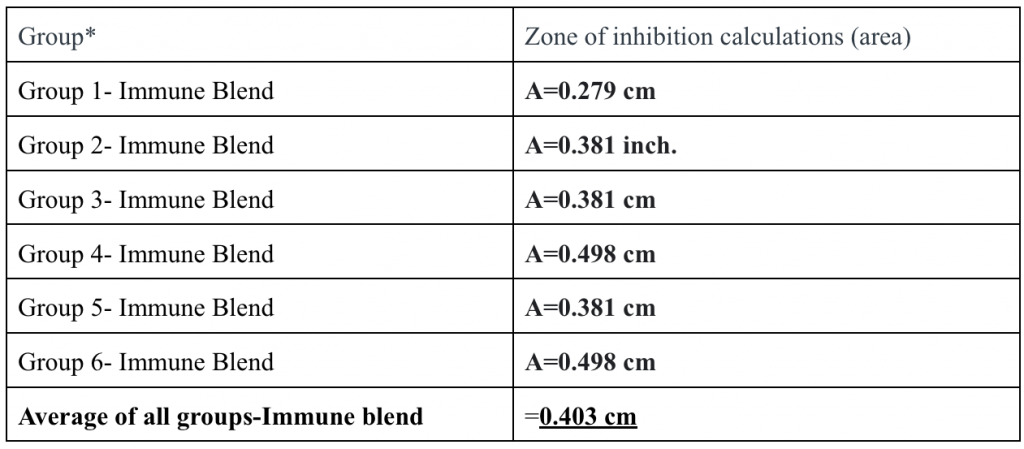
Table 4: Antibiotic+Immune Blend Trials
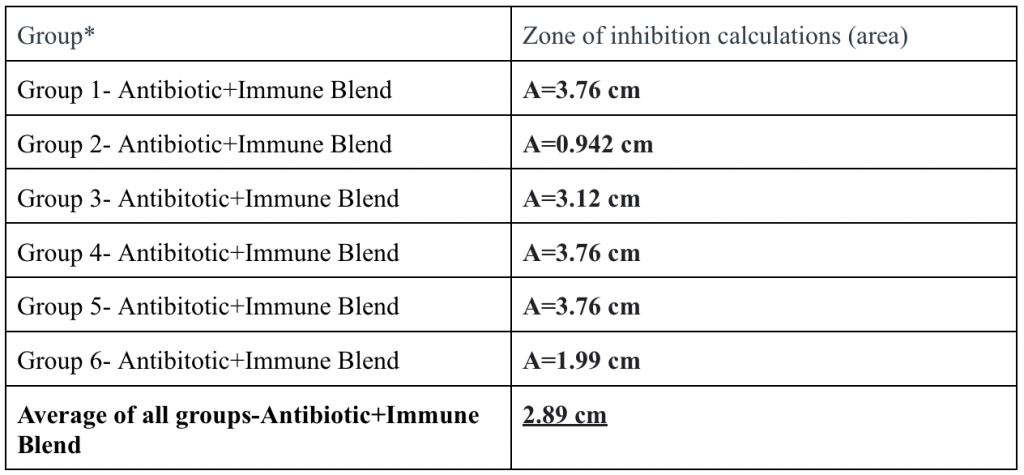
Table 5: Control Trials
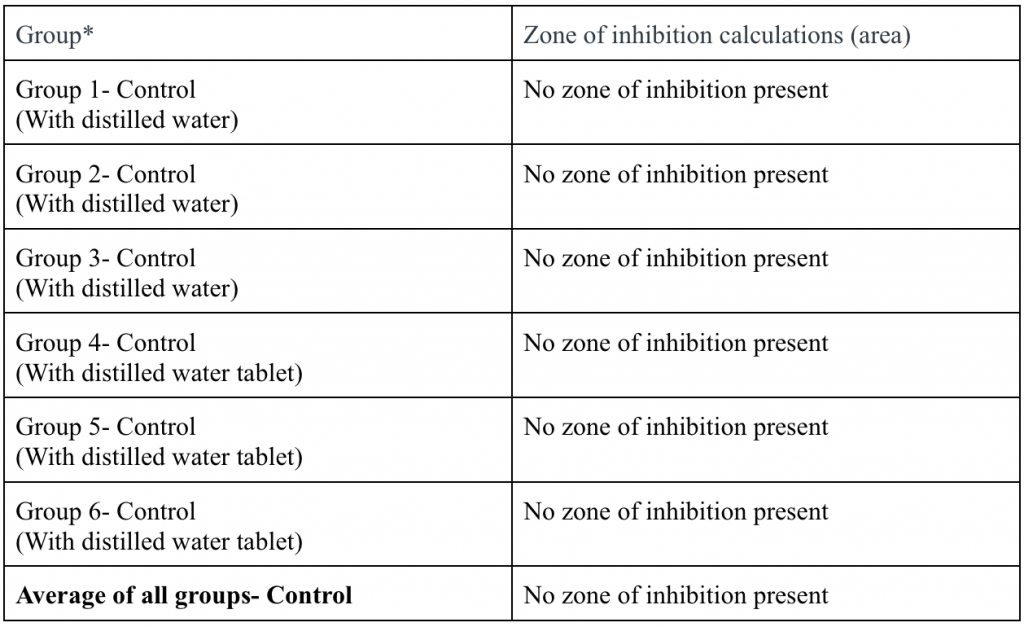
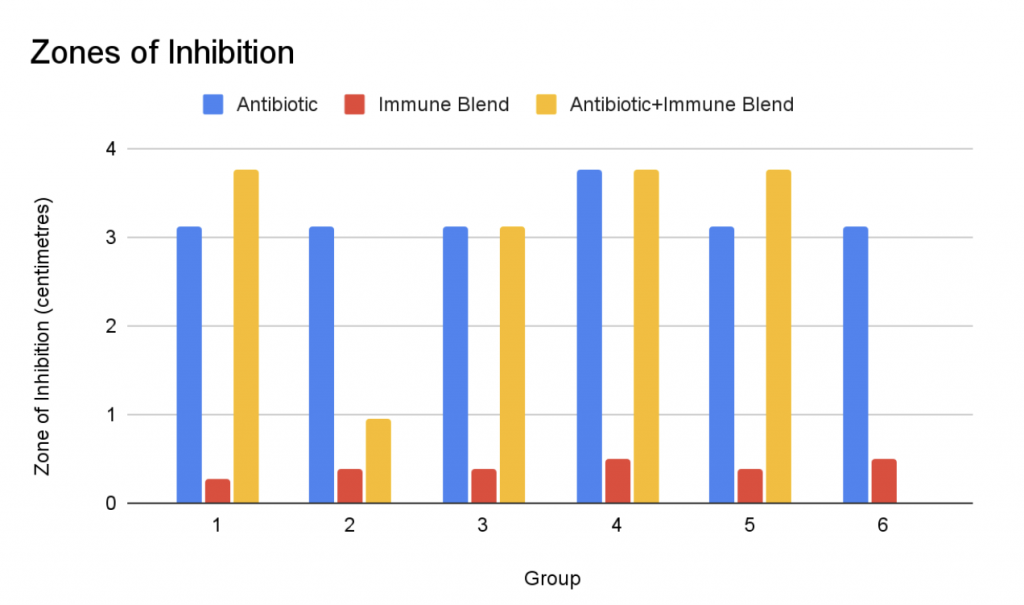
Figure 2: Bar graph representation of the cumulative zones of inhibition
Based on the zones of inhibition and the observations taken, the Immune Blend has antibacterial properties, but does not significantly boost the function of streptomycin. In general, the antibiotic+Immune Blend matched or surpassed the zone of inhibition of the antibiotic. The antibiotic trials produced consistent results, whilst the antibiotic+Immune Blend trials spiked a few different results. In terms of the control group, none of the trials produced a zone of inhibition. Overall, the antibiotic trials had the largest zone of inhibition, being 3.23 centimeters on average. Followed by, the antibiotic+Immune Blend trials with an average zone of inhibition of 2.89 centimeters. Finally, the Immune Blend trials with an average zone of inhibition of 0.403 centimeters.
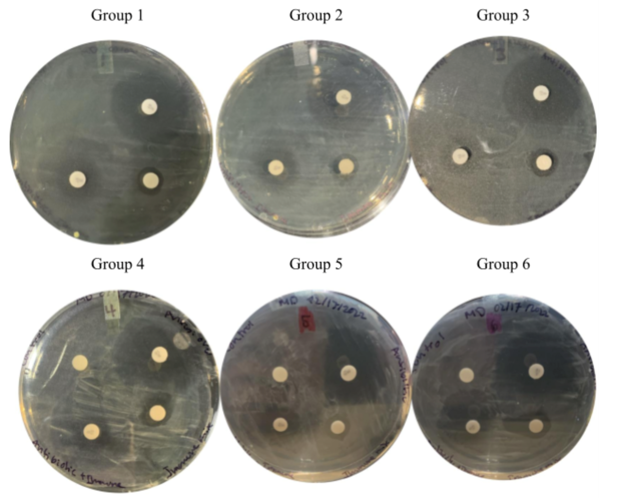
Figure 3: All trials on petri dishes after 1 week in incubator, organized by group
Discussion
The results indicate that the Immune Blend contains some antibacterial properties, but the blend does not significantly boost the function of antibiotics. This paper confirms the antibacterial properties of the Immune Blend because every trial produced a significant zone of inhibition. It is extremely unlikely that the blend drowned out the bacteria because groups 4, 5 and 6 used a sterilized tablet with the same quantity of distilled water as a control. Not a single control group produced a zone of inhibition, which further supports the claim of antibacterial properties being present in the Immune Blend. Additionally, the Immune Blend may not boost the direct function of the antibiotic based on the average results, but the antibiotic+Immune Blend zone of inhibition matched or surpassed the antibiotics zone of inhibition on 4/6 trials.
The lowest antibiotic+Immune Blend zone was 0.403 centimeters compared to the greatest at 3.23 centimeters. It is possible that this trial was a fluke, due to an error that affected the overall average. Furthermore, the zone of inhibition measuring 3.23 centimeters was the biggest zone recorded and it was only observed in the antibiotic+Immune Blend trials. After a week in the incubator, all the antibiotic+Immune Blend zones of inhibition produced a double halo, where the primary halo was very clear and the secondary halo was slightly foggy. It is possible that this is a result of the Immune Blend and antibiotic working together. The primary halo was often the same size as the halo of the Immune Blend trial for each group. This signifies that the primary halo could be the Immune blend at work, whilst the secondary halo is the antibiotic at work. The antibiotic trials produced accurate and consistent results and are an effective way to kill bacteria. The results obtained fit in with similar studies as oregano oil has been claimed to be antibacterial in prior studies. This study supports the claim as the Immune Blend contained antibacterial properties, and oregano oil was a significant component of the blend. Overall, the results obtained point towards the Immune Blend containing significant antimicrobial properties.
A possible source of error could be not mixing the Immune Blend well enough before each use. This error may have affected the antibiotic+Immune Blend and Immune Blend trials because not enough of certain components were used in certain trials. This error may be accountable for the two results that were out of the pattern in the antibiotic+Immune Blend trials. To correct this error in future experiments, the bottle itself should be shaken for one minute before use and mixed with a pipette directly before usage.
Future experiments may try to incorporate different plant extracts, vitamins and minerals which could lead to more antibacterial properties, giving the Immune Blend better results. Prior studies have tested the antibacterial properties of specific plant extracts, such as oregano oil. Finding the top five plant extracts and combining them with vitamins and minerals could create an even more antibacterial Immune Blend .Testing multiple species of bacteria could reveal more accurate results as bacterial infections originate from different species. Specifically, testing gram-positive bacteria would be ideal as the oregano oil used is extremely effective against gram-negative bacteria, so testing the opposite would better represent the overall antibacterial properties of the Immune Blend. Additionally, testing different antibiotics alongside the Immune Blend would be beneficial to determine if the blend could better boost the function of a different antibiotic. The Immune Blend could be given to humans while on antibiotics to determine if the Immune Blend plays a role in healing time. Additionally, clinical trials could determine if the blend helps people beat physical symptoms of infections faster. This Immune Blend has a greater potential that can be discovered through further testing after adjusting or changing variables mentioned above.
References
“Ask the Expert: The Role of Diet and Nutritional Supplements during COVID-19.” The Nutrition Source, 1 May 2020,
www.hsph.harvard.edu/nutritionsource/2020/04/01/ask-the-expert-the-role-of-diet-and-nutritional-supplements-during-covid-19/.
Brad Spellberg, Gail R Hansen. “Antibiotic Resistance in Humans and Animals.” National Academy of Medicine, 22 July 2020,
nam.edu/antibiotic-resistance-in-humans-and-animals/.
Chandra, R K. “Nutrition and the Immune System: An Introduction.” OUP Academic, Oxford University Press, 1 Aug. 1997,
academic.oup.com/ajcn/article/66/2/460S/4655769?login=true.
Masood, N., Chaudhry, A., Saeed , S., & Tariq, P. (2007). Antibacterial effects of oregano (origanum … – probotanic. Retrieved April 1, 2022, from
http://probotanic.com/pdf_istrazivanja/OriganoPDF/origano6.pdf
Pan, Si-Yuan, et al. “Historical Perspective of Traditional Indigenous Medical Practices: The Current Renaissance and Conservation of Herbal Resources.” Evidence-Based Complementary and Alternative Medicine : ECAM, Hindawi Publishing Corporation, 2014,
www.ncbi.nlm.nih.gov/pmc/articles/PMC4020364/.
Ubeda, Carles, and Eric G Pamer. “Antibiotics, Microbiota, and Immune Defense.” Trends in Immunology, U.S. National Library of Medicine, 5 June 2012, www.ncbi.nlm.nih.gov/pmc/articles/PMC3427468/?fbclid=IwAR1Wcmb-nCfKZHZDlUnsWZg8Lfo3QzFibVqbAqJIOuT-EQrYsQ6ZffdGmJ0.
Zusi , K. (2017, November 30). Antibiotics alter the infectious microenvironment and may reduce the ability of immune cells to kill bacteria. Wyss Institute. Retrieved April 8, 2022, from
https://wyss.harvard.edu/news/antibiotics-alter-the-infectious-microenvironment-and-mayreduce-the-ability-of-immune-cells-to-kill-bacteria/